Yemen: A surgeon from Hong Kong in a war trauma surgery hospital

Doctors Without Borders surgical field hospital in Mocha under construction photo was taken July 2018. Following the recent offensive by forces loyal to President Hadi and supported by the Saudi and Emirati-led international coalition on Hudaydah, Médecins Sans Frontières (MSF) has opened a 20-bed surgical field hospital in Mocha, 180 kilometres south of Hudaydah, to respond to increased medical needs. © Nuha Mohammed/MSF
Mocha is an ancient port city on the Red Sea. It’s near the conflict front line, so around 80% of our surgery cases are trauma related, such as gunshot and road accident wounds. Due to limited health care services, the Doctors Without Borders / Médecins Sans Frontières (MSF) emergency surgical centre also takes patients who require life-saving care, such as mothers with childbirth complications and patients with acute abdominal problems.
In the Doctors Without Borders hospital, I worked with four Yemeni surgeons and nine medical doctors. With the heavy load of trauma patients admitted, my colleagues gained experience and improved their trauma surgery skills while I was coaching them.
My role was mainly to assess our staff’s skills and to give advice whenever there might be a better or alternative surgical skill. This involved many surgical subspecialities, including trauma, abdominal, thoracic, orthopaedic, vascular, urological, obstetric and gynaecological surgeries. You might be surprised that we need to cover so many areas of surgery in the settings where Doctors Without Borders works.
Medical skills and expertise available vary from one region to another. In some countries in sub-Saharan Africa, there are just not enough trained medical people compared to the immense needs of communities. Whereas in Middle Eastern countries, there are a good number of quality staff we can find to work with us.
Dr Ryan Ko, a Hong Kong surgeon with Doctors Without Borders, has worked in 15 missions in nine countries. © Dr Ryan Ko

One of the situation at the emergency room of Doctors Without Borders' surgical hospital in Mocha. 12 December 2018. © Agnes Varraine-Leca/MSF
However, chronic and long-term war and conflict limit the development and acquisition of new skills which are essential for medics. The availability and access to medical training is seriously lacking. That’s why capacity building and sharing of our knowledge and experience with our colleagues in the field is one of the less talked about but essential responsibilities of field workers like me being deployed to the field. I felt that surgeons from Hong Kong like me are in a position to impart our expertise, given the standard and quality of skills we have been able to acquire. We can support the aim of ensuring that our fellow medics in war zones can run the hospitals on their own with confidence.
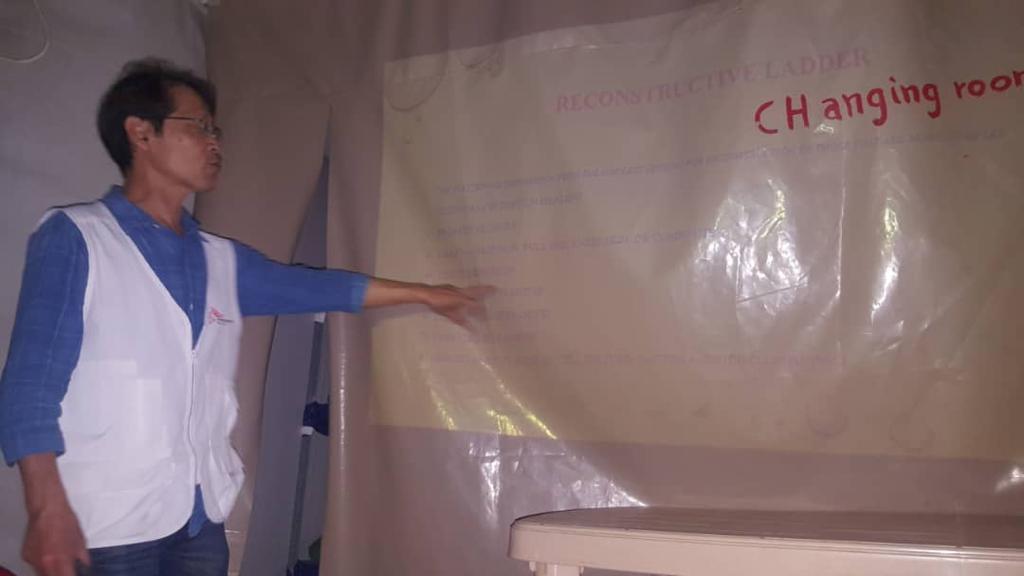
We strive to provide a high standard of medical care. And supporting our colleagues with training, workshops and coaching to upskill them would mean that we could help more patients at a time of distress. So in the three months I stayed in Mocha, I had some very good and friendly knowledge and experience exchanges with my colleagues in every area possible, including wound reconstructive surgery.
This procedure was completely new to them so I needed to train them in a more systematic way. After the training sessions they practice flap surgeries, a technique that is typically used to repair defects left behind after traumatic injury. During my time there, the team conducted 45 flap surgeries which benefitted 42 patients with very good results – shortened hospital stays and fewer follow-ups. The wounds healed well and lots of patients avoided the amputation of limbs, which can seriously affect the mental wellbeing of patients and their loved ones. This procedure would have been especially beneficial to the hospital, given the immense number of trauma patients we saw every day. So this new skill acquired by our surgeons brings relief to patients and also prestige to them as professionals.
At the same time, we built the capacity of the team on diagnostic ultrasound dedicated to identify trauma bleeding in the abdomen and chest. In the surgery world it’s known as extended focused assessment with sonography for trauma (eFAST). In a humanitarian surgery care settings, where patients present with major injuries, this skill can improve decisions on what could be the appropriate course of action for our trauma patients. This capacity building was also extended for our medical doctors, especially for those working in the emergency department where initial assessments of our trauma patients were done.
Within a short period of time, I was very happy to make a difference by imparting my experience and knowledge to our colleagues in the field. They are the staff with the constant presence to care for people and communities in the midst of war and violence.Dr Ryan Ko
I have also shared my perspective as a surgeon on wound management. Since the hospital handles mostly patients who need ongoing treatment of their wounds, it is essential that our teams are able to provide the best care for healing and to prevent the breakdown of skin.
It is equally important for our nurses to be provided with new knowledge. We worked closely with those in our various wards (operating theatre, outpatient, and inpatient) on nursing care for flap surgery. Apart from concepts and theories, whenever I had time I accompanied them in their daily care of these patients.
A Hong Kong surgeon with Doctors Without Borders, has worked in 15 missions in nine countries. Being exposed in various settings and challenges, there is one common issue that communities faced in these areas – big unmet surgical medical needs due to the impact of conflict and war. He worked in Mocha, Yemen from November 2020 to February 2021 to improve the surgical capacity of the team in the newly opened Doctors Without Borders emergency surgical centre.







