India: "My biggest concerns are the knock-on effects of COVID on other aspects of healthcare."
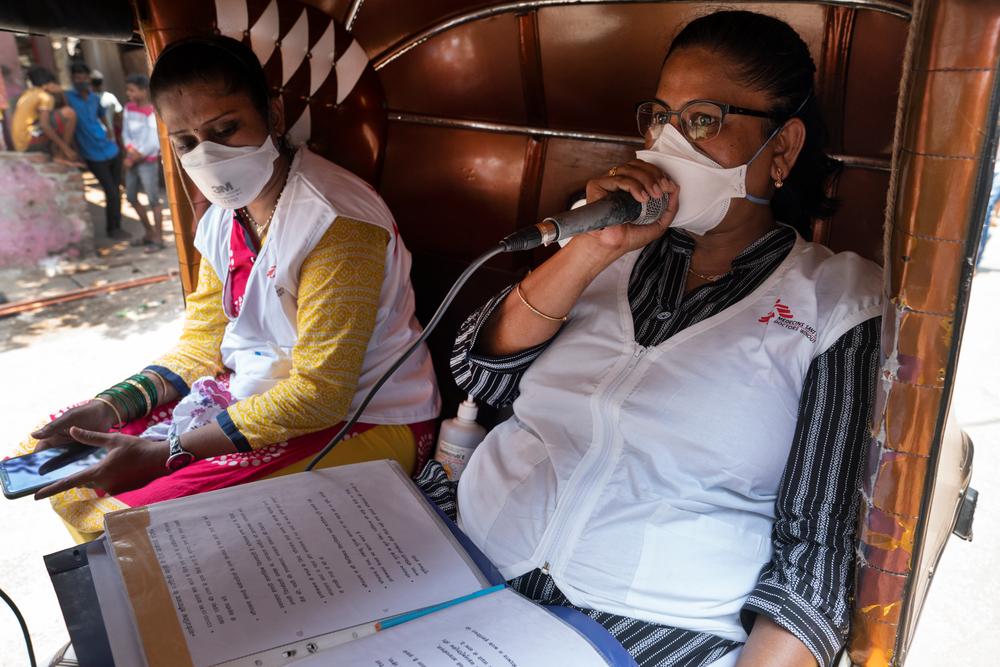
Shagufta Sayyed, Health Educator, making a public announcement on COVID-19 during mass awareness campaign at Industrial pocket in M-East Ward, Mumbai. © Premananda Hessenkamp
In the second wave, there were high number of COVID cases being reported, about 6,000 to 7,000 cases a day which forced authorities to impose a full lockdown. Currently in Mumbai private sector is working from home shops are shut and only essential services are running. The new infections are reduced this week, we are seeing around 3,000 cases everyday right now.
In our independent clinic and the OPD run in collaboration with the National TB elimination programme we’ve adapted to restrictions and for the last three weeks we are only physically present in the clinic on alternate days to see new patients and provide consultations to severely ill. It is important that services are not interrupted for our patients who have a complex f resistant patterns. We’re still diagnosing a lot of new patients with TB who were unable to seek help due to the movement restrictions.
On the other days the medical team works from home carrying out virtual (tele) medical consultations and psycho-social support to our patients by phone. If necessary, they can be prescribed medication on WhatsApp that can be collected from local pharmacies. Otherwise patients can be referred to nearby hospitals for any side effect management or labs for any investigation if needed The community health workers who used do home visits for contact tracing, educating the community about TB are now also following up and providing support over the phone to keep the community and our health workers safe.
Patients who are on TB treatment are familiar with infection, prevention controls (IPC) like wearing masks so they are following these precautions really well. But still when people come to our clinic we’re putting efforts to educate them about COVID-19, we ensure IPC measures are followed with mask wearing and social distancing and we screen and triage patients for COVID symptoms ensuring cases are identified early on. In the first wave, there was much more panic and we saw a lot of fear among patients. Now there are extensive awareness programmes and people are allowed to isolate at home if they test positive for COVID.
Our patient support team is reaching out to our patients over the phone to help them manage their own anxiety and their worries while they’re isolating. Otherwise, if they need oxygen support they are referred to hospital. In our catchment area, there is one designated municipal health facility for isolation of TB COVID-19 co-infected patients and for management of mild and moderate cases. For any severe case management, patients are referred to tertiary care centres. However, the number of critical care isolation bed availability for TB patients with COVID-19 coinfection are very less and need to be available on wider scale, especially for a densely populated city like Mumbai where the TB and DR-TB burden is high.
MoH is trying to do its best but with the load of COVID-19 cases in general, the system is quite overwhelmed, as many health facilities are being converted to COVID-19 care centres, easy access to address other co-morbidities is a challenge.
For patients with lung complications from tuberculosis, there are concerns that they may deteriorate faster. We’re also worried that people may not be accessing TB care because they are scared and worry about what will happen if they get COVID and become serious, and what may happen to their families.Aparna Iyer, Project Medical Referent
Migrant Population
M-East ward where we have our DRTB project is a high burden TB ward and has more than 70% slum population. Many of the patients we treat are migrants who come to Mumbai to look for work and settle down in slums in M-east ward. They are daily wage workers and last year, during the first wave, they were hit particularly hard. Many lost their jobs and were forced to return back home. For people with drug-resistant TB, this meant an interruption to their critical treatment as the drugs they required are often not available in smaller cities or more rural areas. Our patient-support team did try their best to ensure continued care for these patients by linking them to the respective TB treatment centres in their native with the help with the District TB officer and team. However, many couldn’t be reached as their phones were not reachable.
In order to avoid the same situation this year we’re proactively reaching out to our migrant population patients asking them to contact us if they have to leave and let us know where they are going so we can send a supply of medications to their local health centres and get in touch with their local medical teams. We need to ensure a smooth transition and continuity of care for them as they travel home. We’re also offering telephone counselling to try and help with other problems they may face including the loss of work or difficulties obtaining their daily ration support. Our team are offering psychological support and trying find ways to work with other organisations who can help.

Shagufta Sayyed, Community Health Educator, conducting educational talk at the Doctors Without Borders independent clinic in Mumbai, India. © Premananda Hessenkamp
Concerns
My biggest concerns are the knock-on effects of COVID on other aspects of healthcare. Right now, so many hospitals, health care centres and health care workers are being diverted to the COVID response that other vulnerable patients like those with TB, HIV, diabetes or hypertension are having to travel further to find somewhere that can treat them. Currently it’s much harder for them to get the help they need. For example, TB patients would need proper isolation facilities for treatment to ensure infection control.
My main concern is oxygen availability and isolation bed capacity including critical care for DRTB patients co-infected with COVID. What will happen if patients start falling sick when we need bigger capacity for accommodating those with critical needs? If patients are waiting for surgery and they are being deprioritised because COVID has to be dealt with first, then patients waiting for surgery may develop a lot more complications. That is a big concern.






