Innovation: when AI helps improve cervical cancer diagnosis

"Before I started treatment I was in a lot of pain and couldn't eat or sleep at night. Since I have started I feel much better," says a patient during a chemotherapy session at Queen's Elizabeth Central Hospital. Malawi, December 2022. © Diego Menjibar
Cervical cancer is the second deadliest cancer in low- and middle-income countries. In Malawi in East Africa, where Doctors Without Borders / Médecins Sans Frontières (MSF) operates, over 4,000 Malawian women fall sick with cervical cancer every year. With 2,905 deaths due to cervical cancer in 2020, the country also had the second highest rate of mortality.
How can we explain such a high mortality rate from this disease which, in high-income countries, is easily preventable and generally less deadly? The reasons include limited access to prevention and screening, and diagnoses that are not always reliable.
Clara Nordon, Director of the MSF Foundation, has just got back from a visit to Malawi with the Doctors Without Borders teams and tells us about the project led by the Foundation. Code name: AI4CC
Clara, can you "decipher" this internal "code name" and tell us about this emerging project
"Oh yes, we love acronyms at MSF (Doctors Without Borders)! It stands for Artificial Intelligence for Cervical Cancer. The project started three years ago now. The idea was to work on a new, improved protocol for screening cervical cancer.
The goal is to improve cervical cancer screening in order to detect women before they reach the cancer stage and treat them easily. Because yes, when it is detected early, the treatment can be carried out immediately at the health center and is relatively painless and very quick, taking only a few minuts. We must not therefore "miss" these opportunities.
There are three means of doing this: screening more women, earlier and more accurately .
We are thus working on the combined action of a very accurate PCR test affordable enough to be scaled up and better visual assessment through the use of Artificial Intelligence. If we are successful, there is real hope of bringing about genuine change on the ground and saving the lives of many women affected by this disease.
We really need to imagine what it means to live with cervical cancer in Malawi: the lack of treatment options once it develops, the pain it causes, and the repudiation in some cases; it is the entire family unit that is affected in a country where nearly 10% of adults are HIV-positive!"
How can we explain the fact that so many women still die from this cancer in Malawi and in many LMICs, whereas in high-income countries, this disease is easily preventable and generally less deadly?
"Firstly, access to the HPV vaccine remains limited there, even though it is one of the only vaccines that can prevent a cancer, a serious cancer. Secondly, the current screening method, based on a visual evaluation of the cervix, is unreliable. Although this method is inexpensive and has the advantage of being able to be carried out immediately in the health center, it leaves too much room for interpretation and therefore errors. This means that women who have been screened sometimes go home only to come back a few years later with a cancer that can no longer be treated.
The Doctors Without Borders teams really do incredible work in the field and too often have to take care of women for whom treatment options are no longer available. It is also a very heavy burden on the nursing staff.
We needed to find a way to improve this screening strategy and reduce this gap. This cancer is caused by a virus, and we must think of this fight as we think of the fight against an epidemic. Vaccination and diagnosis are our best allies."
How did this project develop?
"Doctors Without Borders, like the rest of the players involved in the prevention and treatment of this cancer, was focused on improving the quality of screening. But when there are disagreements even among the greatest experts, the room for improvement is limited. At the beginning of 2020, the medical division informed us of a study published by the Journal of the National Cancer Institute which highlighted the potential of artificial intelligence in photo analysis for improved detection of precancerous lesions. Based on our experience with Antibiogo, we decided to investigate the potential of AI further. Pauline Choné, a consultant at the MSF Foundation, joined us to begin this work. We contacted the authors, including Mark Schiffman, an expert in molecular epidemiology who has been studying HPV for over 35 years within the NCI! Charlotte Ngo, Doctors Without Borders' oncology consultant, Pauline and I were determined to explore this avenue with them right from the first meeting. When we discussed the Malawi mission, they were also immediately on board. Without them, we wouldn’t be able to do much.
To begin with, we agreed to each rework the algorithm and then compare the results. To do this, we decided to use the bank of cervix images collected by Doctors Without Borders and build an “ideal” annotation tool from the clinicians’ point of view. We formed a partnership with KTH (Royal Institute of Technology in Sweden) and worked for more than a year on this preliminary tool for AI, this key phase is called the annotation of the data set.
When we had finished the annotation tool, the NCI informed us that their algorithm was already complete with results that were conclusive enough to start the validation study. That's also part of innovation! Working for months and not necessarily using the result. The good news was that we were going to be able to move forward faster and potentially be useful in the field more rapidly.
We therefore focused all our efforts on formally building the partnership and linking to Doctors Without Borders in Malawi and Epicentre to the large-scale study that the NCI was preparing: the PAVE study.
This consortium aimed to set up a vast study involving 100,000 women worldwide to evaluate a new approach to cervical cancer screening.
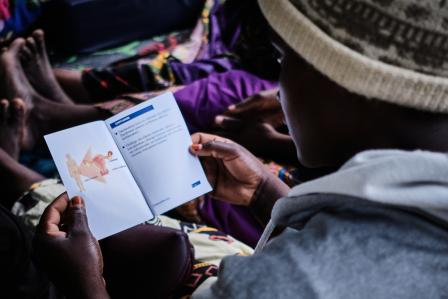
With the help of the Doctors Without Borders teams in Malawi who are on the front line in this project, and upon validation of ethical committees of Doctors Without Borders & Malawian authorities,we aim to include 10,000 women. This cohort will be particularly interesting in this study because we will unfortunately have a high prevalence of HIV-positivity, and therefore potentially results that will also help us improve care for this doubly affected population."
What does this new approach consist of exactly? How will it change the current disastrous situation concerning this cancer?
"This study is based on the introduction of two major innovations:
- Systematic screening via a PCR test, which will triage the women and identify those who are carriers of so-called high-risk HPV (with a high risk of developing into cancer), made possible by a new, faster and less expensive testing technology able to be scaled up by a Health Ministry
- Improved visual evaluation thanks to AI
To do this, during the period of the study, we will do a VIA and keep the photographs of the cervix for HPV+ women and link the status through a biopsy, which is why the mission has equipped itself with a full-scale anatomical pathology laboratory.
The good news is that, even before the results of the study are available, we will provide better screening notably thanks to the systematic PCR test."
Why did the MSF Foundation take up this issue?
"One might think that 4,000 women is "not many", or that this does not represent a sufficiently large-scale action. But when we know that in 2020 almost 3000 women died when this could be avoided, the figure does not matter. And that's also the feedback we were getting from the field: this glaring inequality for these women faced with a disease that was easily preventable elsewhere.
Our role is to act as a researcher, to evaluate what technology can contribute, in a fairly "simple" and direct way, to medical practices in vulnerable environments, and to bring back and adapt practices and tools. Our main work will then be to "set up" a project by drawing on the best resources available both internally and externally. This means organizing a way of working with several groups, from different backgrounds and cultures... towards the same goal. That's also what's so exciting and enriching."
What are the next big steps?
"Our study begins in Blantyre in May 2023. This prospective study will last 12 months and will supply data for the PAVE study. At the end of 2024, the results of the whole consortium’s PAVE study (on 100,000 women) will be known. If the results are conclusive, the NCI will recommend that this new protocol be widely promoted and used in all LMICs. We hope to eventually change the screening protocol in all LMICs, which would have a significant impact on a global level."