Doctors Without Borders is seeing the spread of cholera cases, putting the most vulnerable at risk.
In Haiti, Doctors Without Borders is calling for an immediate intensification of the response to the outbreak; more organisations and donors must be mobilised, and essential tools, such as vaccination, must be made available to medical teams and to people.
Northeast and northwest Syria have been facing a major cholera outbreak since September 2022. First linked to the contaminated water near the Euphrates River and the severe water shortage in the north of Syria, the outbreak has now spread across the country, and more than 13,000 suspected cases have been reported, including 60 deaths (as of 14 October).
Will you support our response?
You can help our works around the world by making a donation today.
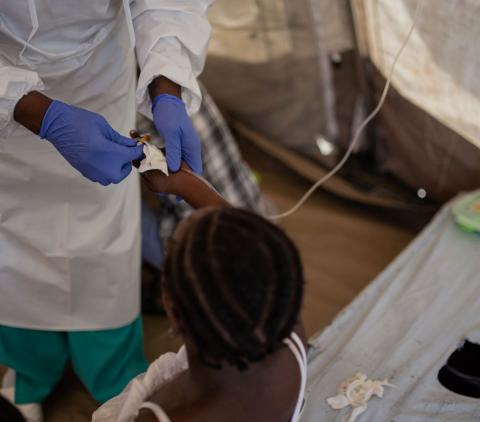
Doctors Without Borders / Médecins Sans Frontières (MSF) often responds to outbreaks of cholera in the countries we work in. But how do we set up our cholera treatment centers to ensure our patients get the best care possible - and that the disease doesn't spread?
How Doctors Without Borders responds to a cholera outbreak
What you should know about cholera
Cholera became a global disease in the 19th century when it spread from its original source the Ganges delta in India. Six subsequent pandemics killed millions across all continents. In 1961, the current (seventh) pandemic started in South Asia, spread to Africa in 1971 and reached the Americas in 1991. Cholera is now endemic in many countries.
According to WHO (World Health Organisation), researchers have estimated that each year there are 1.3 to 4.0 million cases of cholera, and 21 000 to 143,000 deaths worldwide due to cholera.
- What is cholera?
Cholera is an acute infection of the small intestine caused by the Vibrio cholera bacteria. People can get sick when they swallow food or water contaminated with cholera bacteria. Common sources include
- Municipal water supplies
- Ice made from municipal water
- Foods and drinks sold by street vendors
- Raw or undercooked fish and seafood caught in waters polluted with sewage
When a person consumes contaminated food or water, the bacteria release a toxin in the intestines that produces severe diarrhea.
Outbreaks can rapidly spread in over-crowded communities and in dense living conditions when there is inadequate access to clean water, waste collection, and proper toilets. Because of population displacement, destruction of infrastructure, or a lack of public services, cholera is a serious risk in the aftermath of a natural disaster or during a conflict. The situation can be especially problematic in rainy seasons when houses and latrines flood and contaminated water collects in stagnant pools.
- What are the symptoms of cholera?
Symptoms of cholera can begin as soon as a few hours or as long as five days after infection. The infection is often mild or without symptoms, but can sometimes be severe and life-threatening.
Cholera is marked by the sudden onset of profuse, watery diarrhea, which is often accompanied by vomiting.
Patients rapidly become dehydrated suffering from intense thirst and dry tongue. The other symptoms of the infection are rapid heart rate, low blood pressure, muscle cramps and loss of skin elasticity
Children may also experience fever, lethargy, and seizures because of extreme dehydration. The disease ordinarily runs its course in two to seven days.
The rapid loss of fluid from the bowel can, if untreated, lead to death—sometimes within hours—in more than 50 per cent of those stricken.
However, with proper modern treatment, mortality can be prevented, with rates kept to less than 1 per cent of those requiring therapy.
- How is cholera treated?
Cholera is simple to treat in most cases, with people with mild to moderate forms usually able to recover through treatment with fluids and oral rehydration salts, which are easy to administer. People who are severely dehydrated may need intravenous fluids and hospitalisation.
The administration of antibiotics such as tetracycline during the first day of treatment usually shortens the period of diarrhea and decreases the amount of fluid replacement needed. It is also important for patients to resume eating as soon as they can avoid malnutrition or to prevent existing malnutrition from becoming worse.
Without treatment, the mortality rate can reach 50 per cent; with adequate care, it's less than 2 per cent.
- Prevention
A safe and clean supply of water is the key to cholera prevention.
Many effective measures can be achieved by chlorinating public water supplies appropriately and, in some cases, distributing chlorine tablets to households with instructions on how to use them. In the absence of chemical disinfection, people can boil their water before consumption, but this may be difficult to carry out, especially in poor countries.
Hygienic disposal of human waste is also an important measure in preventing Cholera. A latrine can significantly reduce the risk of infection in areas without modern sewerage systems.
Ensuring the safety of food is yet another important control measure.
During an epidemic of cholera, it is important that all food—including leftovers—be thoroughly cooked (to a core temperature of 70 °C [158 °F]) and that it be eaten before it cools. It is also important that stored food be covered to avoid contamination and that people always wash their hands after defecation and prior to food preparation. Foods sold by street vendors have been repeatedly implicated as sources of infection and should therefore be avoided by travelers to areas where cholera is endemic.
Vaccines have been developed against cholera, which supplies protection between six months and three years depending on the type of vaccine and the number of doses administered.
While oral vaccines have proven effective in preventing cholera during outbreaks, the current two-dose strategies are logistically challenging to implement during emergencies. But Doctors Without Borders have seen from previous experience and scientific evidence that a one-dose oral cholera vaccine strategy is not only safe and easy to implement but can also prevent or reduce the transmission of the disease during an epidemic.
- Why are there so many cholera outbreaks today?
In 2022 at least 30 countries have seen outbreaks of cholera or cholera-like diseases. But this is not one big outbreak. For most countries, the current surge of cholera is due to specific, local conditions. The risk factors for cholera outbreaks are well known and always linked to access to clean drinking water and proper wastewater disposal.
Protracted political and/or military crises: this type of crises can lead to a lack of maintenance of drinking water and/or sewage infrastructure. This is the case today in countries like Haiti, Somalia and Syria.
Natural disasters: Heat and drought can reduce the amount of safe drinking water, forcing people to use unsafe sources. Floods on the other hand, can facilitate the bacteria’s spread to previously safe water sources. In 2022, countries like Somalia, Kenya and Ethiopia suffered from severe droughts. Others, like South Sudan and Nigeria, faced floods.
People on the move: Refugees often have to stay in places where there’s not enough access to clean water, and authorities often don’t invest in proper water and waste infrastructure in refugee camps. This year, there were cholera outbreaks in refugee camps in Lebanon, Somalia and Nigeria.
- What are the challenges today?
Cholera is easy to treat, with oral rehydration for most patients, and intravenous rehydration for more severe cases. If treated in time, more than 99% of patients will survive the disease. Providing clean drinking water and correctly processing wastewater protects people from getting infected in the first place. There is also a good vaccine against cholera.
But treatment and prevention of cholera come with considerable logistic challenges. Setting up cholera treatment centres requires a lot of supplies, and so do water and sanitation projects. In places that are unsafe or otherwise difficult to access, that is a huge constraint. And just the number of outbreaks this year makes it very challenging. There’s already a shortage of cholera vaccines and the supply of other essential materials, like the fluid for intravenous rehydration, is also under pressure.
Additionally, sometimes governments don’t want to officially declare cholera outbreaks, often for political reasons. This makes it very difficult to adequately inform the population how they can protect themselves, and impossible to do cholera vaccination.
- What is Doctors Without Borders doing today?
Doctors Without Borders is today running cholera programs in 10 countries (Kenya, Ethiopia, Somalia, Cameroon, Nigeria, Haiti, Lebanon, Syria, Malawi). Our teams are involved in cholera prevention: they do health promotion, water and sanitation works, and cholera vaccination. We’re also running cholera units to treat patients in medical facilities, and have set up bigger, separate cholera centres where hundreds of cholera patients can be admitted simultaneously.
Facts about cholera
Will you support our response?
You can help our works around the world by making a donation today.








