COVID-19 in Papua New Guinea: Supporting self-isolating patients with phone counselling

A counsellor speaks to a patient who is isolating at home. In Port Moresby, Papua New Guinea, the team carries out patient education and counselling to people who tested positive for COVID-19 but show no or light symptoms. These patients may self-isolate at home and are called every other day during the quarantine period to maintain physical and mental health. © Leanne JORARI/MSF
As the coronavirus pandemic rapidly sweeps across Papua New Guinea (PNG), it is inducing a considerable degree of fear and concern in the population at large. This overwhelming concern is largely due to an astounding lack of accurate information about the virus as well as hysteria caused by a whirlpool of conspiracy theories and misinformation. This is resulting in stigmatisation of those testing positive, especially when isolating at home with mild symptoms.
Over 15,000 cases have been registered in the country so far. People who have tested positive for COVID-19 are known to be fearful and anxious, especially considering the stigma associated with COVID-19 in Papua New Guinea. This stigma is mainly based on the fact that it is a disease which is new and unknown. And similarly to many health issues that are unknown, it drives people to hide their illness to avoid discrimination and prevents them from getting tested and seeking healthcare.
We hired and trained new staff members a few weeks back to provide clinical care in Rita Flynn makeshift hospital where COVID-19 patients were treated. But while we started activities, the number of patients needing hospitalisation decreased. The authorities decided to limit COVID-19 care to two other facilities in Port Moresby and closed the ward.Shah Khalid, project coordinator
The Doctors Without Borders / Médecins Sans Frontières (MSF) team is providing patient education and counselling sessions instead. This is carried out over the phone, reaching people in their homes while they self-isolate after testing positive for COVID-19.
The regular phone calls help to check on the status of patients and answer any concerns or questions they have, ensuring the patient’s mental and emotional well-being is not neglected.
Overseeing the tele-counselling is Nurse Benita Apa from the Highlands of Papua New Guinea.
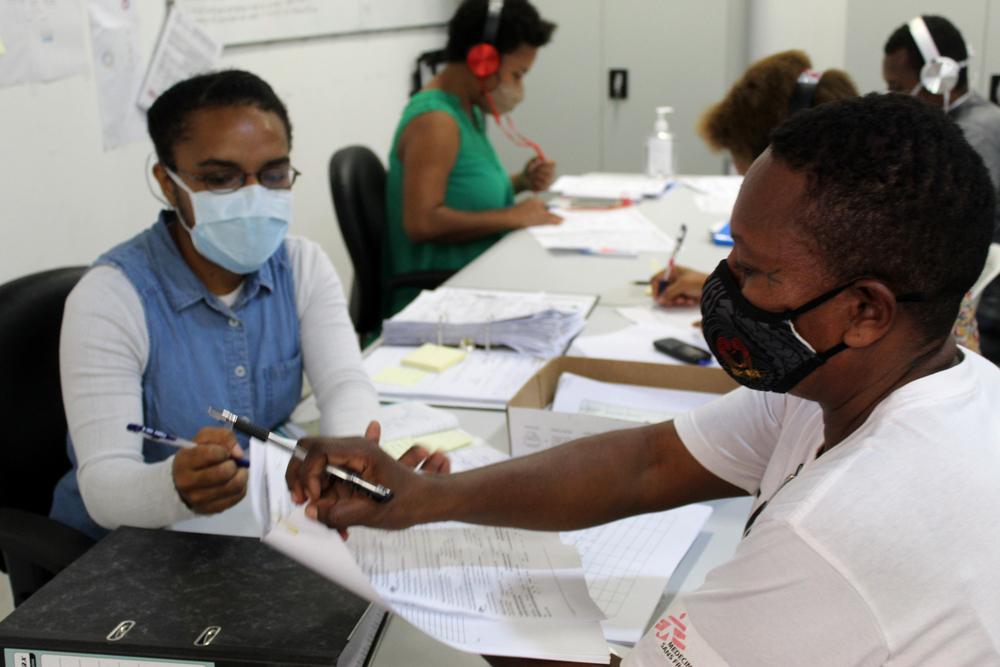
Benita Apa, nurse, explains the patient form to a community health worker. © Leanne JORARI/MSF
Through our tele-counselling sessions we talk to the people who come in and test positive but don’t show severe symptoms; this means they don’t need hospitalisation and can isolate at home. We ask them to provide their phone numbers and then we check on them every second day to ensure their health is stable and most importantly that they are keeping sane and healthy. During this time, their mental well-being can be tested, especially when they can’t go out of their homes or see their friends and family.Benita Apa, nurse
Patients receive information on a healthy diet and how they can practise physical exercise to stay healthy. Up until now, no major issues have been reported by people in home isolation. One man living in a multi-generational household--which is very common in PNG--said that he does his best to stay in a separate room to avoid infecting his family.
The majority of people that the patient education and counselling team contacts are appreciative, but there are others that the team have a difficult time reaching through telephone because they either don’t give their telephone numbers at all or are simply uncontactable. When this happens, it poses a grave problem because there is no other way to communicate with the patients. Community visits have been put on hold because of security concerns and COVID-19 measures enforced by the country’s COVID-19 measures.
