
Breadcrumb
- Home
- What We Do: Providing Mental Health Support
What We Do: Providing Mental Health Support
Doctors Without Borders works in some of the poorest and harshest, sometimes conflict-ridden environments, and in many of these, we have provided comprehensive mental health support to patients for years. From psychological first aid in an emergency setting, to mental health services alongside care for pre-existing conditions and standalone psychosocial and psychiatric care, here are some of the ways our teams respond.
From helping victims of armed conflict to typhoons, we have provided mental healthcare in the Philippines. In 2017, 370,000 people were displaced by the conflict between the Philippine armed forces and two pro-Islamic State factions, the Maute group and Abu Sayyaf, in the Marawi City, Mindanao. We offered psychological first aid to those affected, and have since remained in the area to provide support to internally displaced people and returnees.

In the same year, we responded to the devastation wreaked by Typhoon Tembin in the southern Philippines, offering psychological support, including grief counselling.
In 2020, the restrictions that came with the COVID-19 pandemic led our team to explore new ways to provide mental health support, among which was to provide remote mental health and psychosocial support to persons affected by COVID-19.
"With the stress we face today, the usual coping mechanisms were not enough," said Lyka Lucena, Doctors Without Borders mental health social worker.
Indonesia is located on the tectonic 'Ring of Fire' and is prone to natural disasters. Our team in Indonesia has actively and immediately responded to the natural disasters in the country and provided mental health support to victims, including group mental health counselling.

During the COVID-19 pandemic , our team focuses amongst other on mental health campaigns to support health care workers and the population with coping tools. Dyah Larasati, a psychologist, cautioned that "Burnout can happen when individuals experience extreme emotional, physical and mental exhaustion due to prolonged and excessive stress."
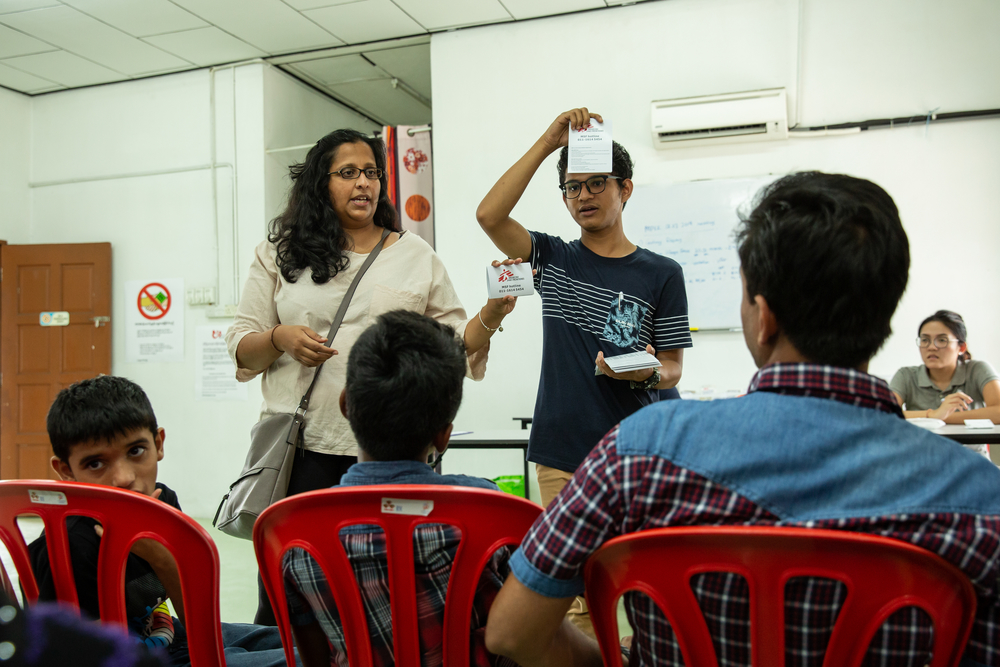
Doctors Without Borders has been present in Malaysia since 2015, to respond to the gaps in access to healthcare faced by refugees and asylum-seekers. Our team, including psychologists and mental health counsellors, provides comprehensive mental health support, including mental health education, psychosocial support and counselling, via community-based mobile clinics and a fixed clinic in Penang, Malaysia.
"On top of the existing struggles of living as a refugee in Malaysia, the secondary impact of this COVID19 pandemic further compounded the already vulnerable mental health condition of this community," said Sarah Chou, mental health activity manager.
In 2020, we worked with R-vision to reach the Rohingya online. R-vision is an online media network in the Rohingya language. We covered COVID-19 prevention measures, explained handwashing, isolation and how people could make their own masks. We also dedicated a video to mental health, reflecting on how people could support each other during the outbreak.

In response to the COVID-19 pandemic, our teams provided face-to-face and virtual health promotion sessions with vulnerable people less likely to access information, such as refugees and domestic workers, and those on the front line, such as street cleaners.
We also created a website to help people manage their stress and worry, which included tips and tools to cope.
In 2020, Doctors Without Borders conducted a total of 349,500 individual mental health consultations.

Are you a mental health specialist? Would you like to help provide mental healthcare?
- Providing mental health first aid
Doctors Without Borders provides psychological first aid to communities experiencing high levels of distress, including in the aftermath of natural disaster. This care provides people with basic support after they have experienced trauma or critical incidents. Community mental health workers or other trained community members can deliver psychological first aid.
In the aftermath of the triple disaster that hit Central Sulawesi, Indonesia in 2018, Doctors Without Borders in cooperation with the Ministry of Health Crisis Centre not only supported health centres in providing basic healthcare and treatment to those injured. We also provided psychological first aid to those who were traumatised by the disaster.
- Trauma counselling and specialised care
Those who have survived extremely stressful situations—refugees, displaced people, disaster survivors, victims of abuse and crime, and survivors or war or genocide—are particularly at risk for severe mental health impacts.
To help heal the patient’s psychological wounds, our mental health specialists listen, support, and train survivors in self-care practices so the traumatic experiences do not come to define their lives. The immediate goal is to reduce their symptoms and empower them to lead happy and healthy lives.
Doctors Without Borders' Mental Health Activity Manager Kathy Lostos who works with Rohingya refugees in Bangladesh says: “The best thing to improve mental health outcomes is to restore a sense of safety. Having some degree of control or autonomy over one's future is a determinant of creating a sense of safety. This includes things like including communities in decision-making processes or creating a sense of autonomy and control over one's future. [This] serves to mitigate the long-term effects of trauma.”
- Mental health support for medical activities
Mental health is an essential component of treatment for HIV/AIDS, tuberculosis, malnutrition, non-communicable disease and surgery and burns patients. During our recent response to the COVID-19 pandemic, our teams have also witnessed the importance of mental healthcare for the recovery of COVID-19 patients.
HIV and tuberculosis patients must endure lengthy and gruelling treatment plans; for people with these and other chronic health conditions, or contagious diseases like Ebola and Lassa fever, there is also economic stress, loneliness and stigma, and sometimes psychiatric side-effects from medication. Adherence counselling can help patients to stick to their treatment and cope with the challenges they face in living with and tackling their illness.
Children who are malnourished face the risk of delayed development, and mental health treatment can help support them as well as their caretaker, who may also be experiencing a mental health disorder.
- Local and culture specific responses
When our mental health teams begin work in a new community, one of their first steps is to seek out local leaders who can guide the team on the strategies that will best match people’s needs. Communities often need to rebuild themselves as a whole to help strengthen the identities of the people within them.
In many cases, our mental health staff are from the communities being assisted. Their knowledge and understanding of their community’s experiences, as well as values and practices around mental health, are very beneficial to providing effective treatment.
Our holistic approach to healthcare
Doctors Without Borders provide mental healthcare both as an integrated part of medical activities and as standalone mental health projects.
Our teams aim to alleviate people’s mental suffering, enhance their functioning and respect their dignity, utilising a combination of a holistic approach to clinical care and community-based activities. Often this work is carried out by local counsellors trained by our teams at Doctors Without Borders, with psychologists or psychiatrists providing technical support and clinical supervision.
When appropriate, our counselling services may reinforce or complement mental healthcare approaches that already exist in the local communities where we work. It is important that our approach to mental healthcare includes local and culturally-specific definitions and perceptions of psychosocial health.