Latest update
Tuberculosis (TB) is the world’s deadliest infectious disease. In 2021, 4.2 million people with TB were not diagnosed—more than 1 in 3 people with TB. Without proper diagnosis, people with TB can’t get the treatment they need.
Doctors Without Borders / Médecins Sans Frontières (MSF) is calling on US-based diagnostic corporation Cepheid and its parent corporation Danaher to prioritise people’s health over profits, and reduce to the price of its GeneXpert tests to $5.
In the last decade, rapid molecular tests such as Cepheid’s GeneXpert have revolutionised TB diagnosis, and are now recommended by the World Health Organization. But high prices and intellectual property barriers continue to hamper the uptake of these tools by countries.
The “Time for $5” campaign calls on US-based diagnostic corporation Cepheid and its parent corporation Danaher to prioritise people’s health over profits, and reduce to the price of its GeneXpert tests to $5.
Cepheid’s GeneXpert diagnostic testing technology has revolutionised rapid, accurate, near-point-of-care diagnosis of tuberculosis (TB), the deadliest infectious disease in the world, as well as HIV, Ebola and hepatitis C, among other diseases. Doctors Without Borders / Medecins Sans Frontieres uses these tests routinely in medical programmes around the globe.
Due to the high price of the GeneXpert test cartridges, many LMICs cannot scale up testing for all people who need diagnosis. Doctors Without Borders analysis has shown that it costs Cepheid less than $5 to manufacture one GeneXpert test, but Cepheid charges Doctors Without Borders and LMICs at least 2 to 4 times that price, depending on the disease.
We need these prices to go down now.
What is tuberculosis?
Tuberculosis (TB) is an infectious disease caused by a bacterium called Mycobacterium tuberculosis that mainly affects the lungs.
When someone who is sick with TB disease of the lungs or throat coughs, speaks, laughs, sings, or sneezes, the TB bacteria passes from them through the air. When another person breathes them in, the bacteria can settle in the lungs and begin to grow.
People with TB disease are most likely to spread it to people they spend time with on a daily basis, such as family members, friends, and co-workers or schoolmates.
Anybody can get tuberculosis.
Did you know? Tuberculosis kills at least 1.5 million people each year*. It was the deadliest infectious disease in the world before COVID-19 occurred. During the COVID-19 pandemic, the number of TB-related deaths rose, and the number of new TB cases increased for the first time in decades.
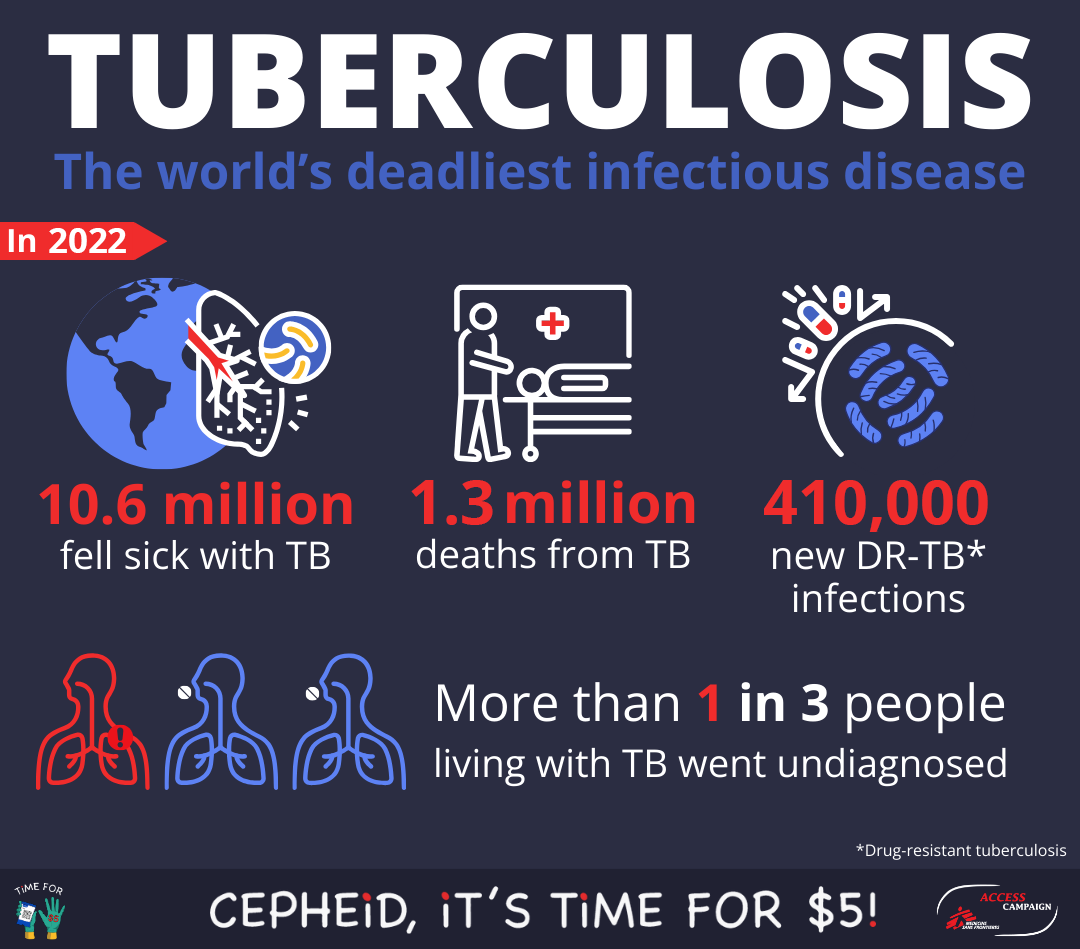
In 2022, an estimated 10.6 million people fell ill with TB worldwide: 5.8 million men, 3.5 million women and 1.3 million children. TB is present in all countries and age groups.
In 2022, 1.3 million children fell ill with TB globally. Child and adolescent TB is often overlooked by health providers and can be difficult to diagnose and treat.
In 2021, the 30 high TB burden countries accounted for 87% of new TB cases.
Worldwide, TB is the second leading infectious killer after COVID-19, killing more people than HIV/AIDS.
TB is curable and preventable.
US$ 13 billion is needed annually for TB prevention, diagnosis, treatment and care to achieve the global target agreed at the 2018 UN high level-meeting on TB.

In 2022, 17,800 people in the care of Doctors Without Borders around the world were started on TB treatment, including 2,590 people with DR-TB. We are working closely with national TB programs, ministries of health, and other key stakeholders in our various projects around the world to ensure access to TB treatment.
What is Doctors Without Borders doing about tuberculosis?
Doctors Without Borders has been involved in tuberculosis care for over 30 years and opened its first programmes to treat multidrug-resistant TB in 1999. Doctors Without Borders has TB treatment projects in 30 countries; it is one of the largest non-governmental providers of treatment for drug-resistant TB.
The settings in which Doctors Without Borders provides TB care vary widely. They include countries with overburdened health systems such as Papua New Guinea, urban slums in the Philippines, and countries with insecure contexts such as Myanmar and Afghanistan.
- Philippines
More than 650,000 people live clustered in Tondo, an area of about nine square kilometers stretching between the port and the business district of Manila. It is one of the most densely populated slums in the world. For nearly two years, strict anti-COVID-19 measures contributed to overcrowding, with neighborhoods and homes completely confined, and no one allowed out for days at a time.
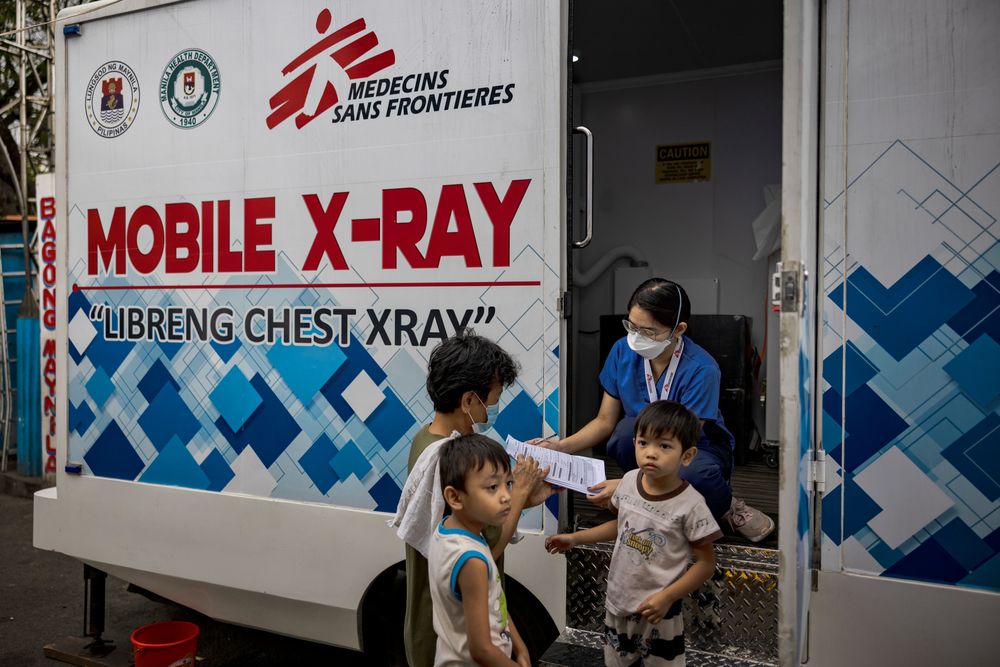
Doctors Without Borders launched a TB active case finding project in collaboration with the Manila Department of Health. Since May 2022, Doctors Without Borders teams have been visiting the different barangays (neighborhoods) of Tondo with a mobile x-ray truck. The aim is to make screening accessible and available as close as possible to where community members live and work. As of March 2023, the project has screened a total of 22,631 patients, and 4.6% of all of the people have been found positive on GeneXpert for TB.
- Papua New Guinea
Papua New Guinea (PNG) has one of the highest prevalence rates of tuberculosis (TB) in the world with 30,000 new cases reported every year, according to the World Health Organization. The high prevalence is such that the PNG government has declared a state of emergency in several provinces.

Doctors Without Borders has been supporting TB care in PNG since 2014. In collaboration with the national TB programme, our team has been scaling up the capacities for screening, diagnosis, treatment initiation and follow-up in Port Moresby’s Gerehu hospital. Mobile teams work in the community to improve patient adherence to treatment.
In Gulf province, our TB programme supports two health centres as well as Kerema general hospital.

- Ukraine
In Zhytomyr, Ukraine, our teams works with the Regional TB Dispensary to treat patients who have drug-resistant forms of tuberculosis (DR-TB). They are treated with a short course of DR-TB medication and the possibility of being treated at home most of the time; meaning patients can get back to their lives, families and careers sooner. Yet, completing the new treatments can still be tough.

Doctors Without Borders nurse Oleksandr Oleksandr Vovkogon observes Vitalii Gorbachov, 56, as he takes his DR-TB pills – most patients in this programme can be treated with an all-oral course of medication instead of the painful injections that were previously used and caused serious side-effects. Ukraine, June 2021. © OKSANA PARAFENIUK/MSF
Patients face practical challenges. In our programme, patient support teams (nurses and social workers) work with DR-TB patients to understand and resolve potential barriers to completing treatment, from unpaid pensions to a lack of gas or heating in their homes.
Coordinated patient support – including doctors, nurses, TB specialists, psychologists and social workers – should be a central part of their treatment.
- Myanmar
Myanmar is still one of the 30 countries with a high TB burden and bears a triple burden of drug-susceptible TB (DSTB), drug-resistant TB (DRTB) and HIV-associated TB.
Doctors Without Borders has been involved in TB care in Myanmar since 2002. Progress was made tackling this infectious disease until 2019 but the combination of Covid-19 and the collapse of the healthcare system due to the military takeover stalled and reversed this improvement in 2020 and 2021. 60,000, people with TB were estimated to have gone undiagnosed and untreated during this period, increasing TB related deaths, more TB transmission and more people developing resistant forms of TB.

In 2022, 33 people were started on treatment for MDR-TB. In 2023, official data from the National Tuberculosis Programme (NTP) shows that testing and identification of TB in Myanmar is reportedly moving back towards WHO targets. The data mostly represents the Yangon Region, which is where 50% of the TB burden in Myanmar comes from.
Since Doctors Without Borders started supporting the National Tuberculosis Reference Lab in 2021, we have seen a steady increase in the amount of testing that is performed monthly, with most samples coming from the Yangon Region.
Our teams in Myanmar are providing regular support to NTP programmes at different levels, either supporting direct service provision (like in Yangon) or facilitating access to testing and treatment (like in Kachin, Shan and Rakhine).
- Afghanistan
In Afghanistan, people often struggle to afford even basic food items, let alone travel expenses and medical fees for hospital visits. Meanwhile, the public healthcare system is under-resourced, under-staffed and under-funded.
The Doctors Without Borders TB hospital in Kandahar is the only medical facility providing advanced TB care in southern Afghanistan. Many of our patients come from the nearby provinces, but others travel from up to 350 kilometres away. “We support them by paying for transport costs, housing expenses and food to alleviate some of the economic burden,” says Doctors Without Borders medical advisor Allieu Tommy. Without such incentives, most patients could not afford to come for treatment.
Difficulties reaching and affording medical care are not the only barriers to TB treatment faced by people in Afghanistan. Another is the widespread lack of knowledge about the disease. Our teams carry out regular health promotion activities in local communities in Kandahar to improve people’s understanding of TB. We also provide information about TB to patients and caretakers at the hospital in Kandahar.

Doctors Without Borders nurse Aziza Khushal waits to collect a sputum sample from a new patient on the women’s side of the Doctors Without Borders drug-resistant tuberculosis hospital in Kandahar city. Afghanistan, March 2022. © LYNZY BILLING
Some patients have a form of the disease that is resistant to conventional TB drugs and require treatment that lasts from nine to 12 months. This can be especially difficult to cope with whilst in a hospital and far from friends and relatives. As a result, many patients fail to see their treatment through to the end. But in 2023, following research results, a six-month short course regimen will be introduced that should make it easier for people to finish their treatment.
Doctors Without Borders has already set up a DR-TB programme that combines specialist inpatient care with supervised home-based treatment to help patients better cope with the regimens.
Innovating and advocating for TB
In addition to providing care, Doctors Without Borders also supports TB research and clinical trials, such as the endTB clinical trial.
- endTB Clinical Trials
Roughly half a million people fall sick with MDR/RR-TB each year, and many die from it.
MDR/RR-TB is a disease caused by a TB bacterium that is resistant to rifampicin, one of the most powerful first-line antibiotics, plus/minus resistance to isoniazid. Roughly half a million people fall sick with MDR/RR-TB each year, and many die from it. Though a range of MDR-TB regimens are now in use around the world, many people are still treated with conventional treatments that are long (up to 24 months), ineffective (only 59% treatment success in 2018), and often cause terrible side effects, including acute psychosis and permanent deafness.
Patients on these regimens must ingest up to 14,000 pills over the full course of treatment, and some have to endure months of painful, daily injections.

The endTB regimens represent important alternatives for short MDR-TB treatment and complement the use of another highly effective, shorter MDR-TB regimen, called BPaLM, which is not suitable for certain populations. The endTB trial results were presented at the Union World Conference in France, in November 2023. The results revealed evidence to support the use of four new, improved regimens to treat multi-drug resistant tuberculosis or rifampicin-resistant tuberculosis (MDR/RR-TB). The team—led by Doctors Without Borders / Médecins Sans Frontières (MSF), Partners In Health (PIH), and Interactive Research and Development (IRD) and funded by Unitaid—formed the endTB consortium and began this Phase III randomized controlled trial in 2017.







